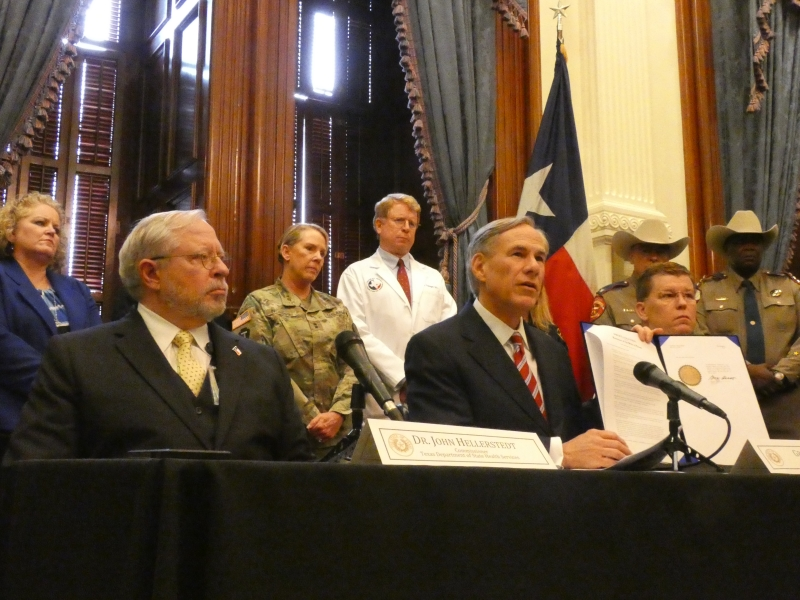
Two years ago this week, normal life in Texas stopped. Uncertainty, fear, and anxiety loomed as the new coronavirus, SARS CoV-2, arrived in Texas. Looking back, physicians reflect on the ongoing impact of March 13, 2020, when Gov. Greg Abbott declared a state of emergency due to COVID-19, the disease the virus causes.
Nearly 100 Texans already were infected by the virus by that week, and one Texan had died.
“I definitely did not think this would be something that would sweep over the globe, sweep over the United States, sweep over everywhere,” said Ogechika Alozie, MD, an El Paso infectious disease specialist and a Texas Medical Association (TMA) COVID-19 Task Force member.
COVID-19 did sweep everywhere. In two years, Texas has confirmed nearly 5.5 million cases of COVID-19. The virus has claimed more than 85,000 Texas lives.
Physicians and public health professionals urged everyone to quarantine to stop the virus’ spread. People packed up their desks and began working remotely. The governor mandated everyone to stay home.
Physicians and nurses stayed on the front lines, however, fighting the virus every day without vaccines or therapeutics. Some were concerned for themselves and their families.
“My biggest fear was dying. It was all you heard of in the northeast – doctors dying, nurses dying, people dying, long lines at hospitals,” said Dr. Alozie.
PPE miracle
Physicians soon faced an onslaught of patients sick from the highly infectious virus, though insufficient personal protective equipment (PPE) – gloves, masks, gowns, and the like – left them somewhat defenseless.
“Early on the lack of PPE was appalling,” said David Fleeger, MD, who was TMA president when COVID-19 first hit. “Doctors and staff were reusing N95 masks over and over.”
He saw physicians wear trash bags as makeshift protective gowns, while others tried to buy PPE from overseas or used homemade masks. The state of Texas was amassing PPE to help frontline workers, but doctors in clinics were doing without; Dr. Fleeger realized the state’s efforts were aimed at helping hospitals.
“Private practice physicians weren’t even on their radar,” he said.
Through TMA and county medical societies, Dr. Fleeger helped urge the state to help redirect PPE to community physicians. TMA set up a statewide distribution system for the state-acquired PPE. Ultimately, TMA and county medical societies sent tens of millions of masks to physicians across the state.
“What should have taken weeks or months took only days. What seemed impossible became a miracle,” said Dr. Fleeger.
Pushed to the brink
Physicians have since faced multiple COVID-19 surges, working extended shifts and fighting fatigue as hospitals filled with patients.
Early on, “almost every room in the [emergency department] was occupied by a patient with COVID-19, and of course, we ran out of rooms to keep patients,” said Diana Fite, MD, a Houston-area emergency physician and TMA’s second pandemic-era president.
El Paso was among the nation’s worst-hit areas during the first COVID-19 surge. More than a thousand patients were hospitalized there every day.
“We did not have space in the hospitals, we did not have nurses, we had doctors that were getting sick, and that’s when we were putting tents outside the hospital,” said Dr. Alozie.
The situation was so dire officials erected mobile morgues to store bodies. “That was a surreal experience,” he said. “I would never want to go back to that period in time.”
As physicians and health care workers fought to keep hospitalized patients alive, telemedicine thrived as a contactless means of taking care of everyone else. Meanwhile, doctors waged another battle, against misinformation and distrust of the medical profession.
“The public had the impression in the beginning that a lockdown would only be needed for two weeks, and when that proved false, a lot of people started losing trust,” said Dr. Fite.
Vaccines key to “normalcy”
Some of that mistrust lingers today, although physicians have more data and knowledge about preventing and fighting the virus, vaccines are widely available, and there are monoclonal antibody treatments and drugs to treat sick patients. Thanks to those scientific developments, COVID-19 cases have declined even though the virus is still present. Fewer than 2,000 Texans are hospitalized with COVID-19, a fraction of the more than 13,000 Texans who were hospitalized just six weeks ago.
TMA physicians and others continue to urge everyone to get vaccinated as the best way to return to some sense of “normalcy.”
“Those who are unvaccinated are always going to be at risk for long-term and severe complications from COVID,” said Dr. Alozie.
Though COVID-19 vaccines are easy to find, some people still refuse to get the shot – although unvaccinated people are more than 65 times more likely to die of a COVID-19-related illness than people up to date with vaccines including a booster dose. More than 60% of Texans aged 5 and up are fully vaccinated (have completed the primary vaccination series), and about 36% of those eligible also have received their booster shot, according to data from the Centers for Disease Control and Prevention.
Along with a need for better vaccination rates, physicians say the pandemic confirmed the need for strong public health infrastructure.
“I am hopeful that lessons have been learned and locked in so that future generations don’t repeat our mistakes,” said Dr. Fleeger.
TMA is the largest state medical society in the nation, representing more than 56,000 physician and medical student members. It is located in Austin and has 110 component county medical societies around the state. TMA’s key objective since 1853 is to improve the health of all Texans. TMA’s Vaccines Defend What Matters initiative helps Texans make informed vaccination decisions for themselves and their families.